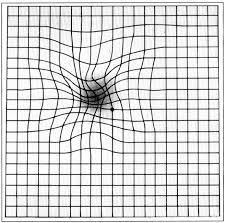
Macular degeneration distorts the center of an Amsler grid
Age-related macular degeneration (AMD) is a major cause of vision loss in people over 50. Thirty percent of us will develop it by age 75-85. There is no cure. For the 10% of patients with wet AMD there are several mainstream treatments that can slow progression of the disease, including drugs injected into the eye, photodynamic therapy, and laser surgery. For dry AMD, which affects 90% of patients, there is only one evidence-based treatment and it is based on somewhat questionable evidence: the Age-Related Eye Disease Study (AREDS) found that a mixture of dietary supplements could slow the progression of moderate to severe disease, but the results may have been misreported and may actually have been negative.
In the world of real medicine, researchers are investigating promising stem cell treatments. In the world of not-so-real medicine, enthusiastic but unsupported claims abound. I recently wrote about a claim that the Santa Fe acupuncture protocol would reverse macular degeneration in four days. The notorious Natural News website claims that saffron cures macular degeneration. I wish! Bogus stem cell clinics in foreign countries encourage stem cell tourism and hundreds of clinics in the US offer their own untested versions of stem cell treatments. I recently wrote about a Pain Relief Center that offers stem cell treatments that may not even contain stem cells.
A recent issue of The New England Journal of Medicine (NEJM) contained five articles about stem cells: two Brief Reports, the first about a successful intervention, the other about interventions that left three women blind, an editorial about those two Brief Reports that called them “Polar Extremes,” an article in a series on Clinical Implications of Basic Research about reprogramming stem cells in vivo, and a Perspectives article from the FDA about “Clarifying Stem-Cell Therapy’s Benefits and Risks” that addresses regulatory issues.
Background: Basic research
Embryonic stem cells are pluripotent cells in the embryo that produce all the different cell types and organs of the fetus. If we could understand how they accomplish that, we might be able to use that knowledge to heal injured tissues or even build whole new organs. Stem cells hold great promise, but research using embryonic stem cells has generated moral objections and regulatory restrictions, and researchers looked for ways to study the processes without using human embryos.
Non-embryonic stem cells can be found in cord blood, amniotic fluid, and various adult tissues. They are multipotent rather than pluripotent (they can’t develop into all types of cells). They are typically found in small numbers and are difficult to process. They have produced some sporadic successes but have been associated with serious complications and there is concern that they might cause cancer.
In 2006, there was a breakthrough. Researchers in Japan (Takahashi et al.) succeeded in reprogramming adult human skin fibroblast cells into a pluripotent state by treating them with four defined transcription factors: Oct3/4, Sox2, Klf4, and c-Myc. These induced human pluripotent stem cells (iPSCs):
were similar to human embryonic stem (ES) cells in morphology, proliferation, surface antigens, gene expression, epigenetic status of pluripotent cell-specific genes, and telomerase activity. Furthermore, these cells could differentiate into cell types of the three germ layers in vitro and in teratomas.
Scientists are developing techniques for guiding iPSCs to differentiate into specific cell types in the lab. On a lab tour during a medical school reunion at the University of Washington, I got to see a Petri dish containing beating human heart cells that had been derived from adult human skin cells! I was very impressed; it was hard to believe it wasn’t science fiction. The hope was that they could be generated from the skin of a patient who had had a heart attack and injected into the damaged area of heart muscle to regenerate it. Since they were derived from the patient’s own cells, rejection would not be a problem; but there were other challenges like the development of tumors, karyotypic instability with long-term culturing, the development of an immune response even to the patient’s own cells, immature phenotypes (more like fetal heart cells than adult ones), heterogeneity of heart cell subtypes, and difficulties in scaling up to large quantities.
They thought some of these problems might be avoided by generating the iPSCs in vivo, in the patient’s body, rather than in vitro in cell cultures in the lab. They developed a procedure to do that in mice, but the mice developed teratomas (tumors comprised of tissues not normally found in the tumor’s location).
The next step was to investigate partial reprogramming in vivo, inducing undifferentiated cells that are not yet iPSCs. These cells transiently express the four transcription factors, but then they redifferentiate into normal functional cells. Short bursts of partial reprogramming improved multiple age-related degenerative processes in mice without producing teratomas.
An example of meticulous science
A group of researchers in Japan surgically implanted an iPSC-derived sheet of retinal pigment epithelial (RPE) cells under the macula to treat a 77-year-old woman with macular degeneration. They proceeded with what the NEJM editorial characterized as “care and prudence.” They only treated one eye. The study protocol was approved by institutional and ethical review boards, reviewed by the Committee on Science and Technology of Health Sciences Council, and approved by the Minister of Health, Labor, and Welfare. The study was performed in accordance with the Declaration of Helsinki, and written informed consent was obtained.
Before transplantation, they took extraordinary precautions. They studied the cells to ensure that they had the same DNA methylation and gene expression profiles as RPE; they gave them to immunodeficient mice to make sure they didn’t cause tumors; they did whole-genome sequencing to ensure that there were no single nucleotide variations that had been reported as cancer driver mutations; they screened for DNA copy number alterations, insertions, and deletions; and they confirmed that plasmid DNA was not inserted into the genomic DNA. They rejected a second cell line that did not meet their criteria, and they decided not to treat a second patient because they had concerns about the genetic integrity of his iPSCs; they found three aberrations in his DNA copy numbers that might affect gene expression, and there were other concerns.
The treatment stabilized the patient’s vision and there were no serious complications.
The polar extreme: wanton misapplication of cellular therapy
In stark contrast, three elderly women were treated with intravitreal injections of a slurry derived from the patients’ adipose tissue, harvested by liposuction. Such treatments have been used experimentally to treat a number of conditions, from sports injuries to Crohn’s disease and spinal cord injuries; and they have been associated with serious complications. The three patients were treated at a stem cell clinic that had an institutional review board approved research trial listed on ClinicalTrials.gov, but the written information provided to at least one of the patients did not mention participation in a clinical trial. Nevertheless, that patient believed she was enrolled in a clinical trial. All three women paid $5,000 each for the treatment; patients in clinical trials are usually not charged and may even be paid for participating. They treated both eyes at once, which I think was a terrible mistake. In an experimental procedure like this, something may well go wrong; and if vision is lost in the treated eye, it would be good to have an untreated eye that was not affected.
The results were catastrophic. Patient 1 started with a visual acuity of 20/60 and 20/30 and ended up with no light perception at all in either eye. Patient 2 went from 20/50 and 20/100 to 20/200 and ability to detect only hand motion. Patient 3 went from 20/40 and 20/200 to ability to detect only hand motion in one eye and light perception only in the other eye. All three patients developed a lens subluxation in one or both eyes; two had intraretinal hemorrhages, two developed macular thickening, and all three had retinal detachments in both eyes.
Regulatory concerns
Three doctors from the FDA spoke out in an article in the Perspectives section of the NEJM. They are concerned that:
…hematopoietic stem cells and stem cells derived from sources such as adipose tissue are being used to treat multiple orthopedic, neurologic, and other diseases. Often, these cells (whether derived from autologous or allogeneic sources) are being used in practice on the basis of minimal clinical evidence of safety or efficacy, sometimes with the claim that they constitute revolutionary treatments for various conditions.
One of the biggest questions in stem cell research is whether the stem cells will get to where we want them to go and do what we want them to do. Some providers assert that stem cells can sense their environment and can detect what deficits are present and do whatever is necessary to correct them. That claim is not based on any scientific evidence.
The authors say:
Claims that therapies are safe and effective must be based on evidence. Standards of evidence help keep unsafe or ineffective therapies out of routine use, while permitting adoption of therapies with a favorable risk–benefit balance.
They point out that there is no reporting requirement for adverse effects outside of clinical studies, so adverse effects of stem cell treatments may be more common than we realize.
Stem cell research involves unique challenges. The FDA is committed to working with investigators to build up the scientific foundations of stem-cell treatments, to make effective treatments available without undue delay while protecting patients from harm. They point out that for serious and life-threatening diseases in which there is an unmet medical need, expedited pathways are readily available. In 2016, the International Society for Stem Cell Research (ISSCR) published guidelines for research.
Conclusion: Unproven stem cell treatments should not be offered outside of clinical trials
In the NEJM editorial, the authors concluded:
The provision of autologous cellular “therapies” outside the experimental clinical trial setting — and on a for-profit basis — is a gross violation of professional and possibly legal standards; it carries the risk of worsening human health and violates the long-standing medical tradition of primum non nocere.
I couldn’t agree more.
